What is Abdominal Pain?
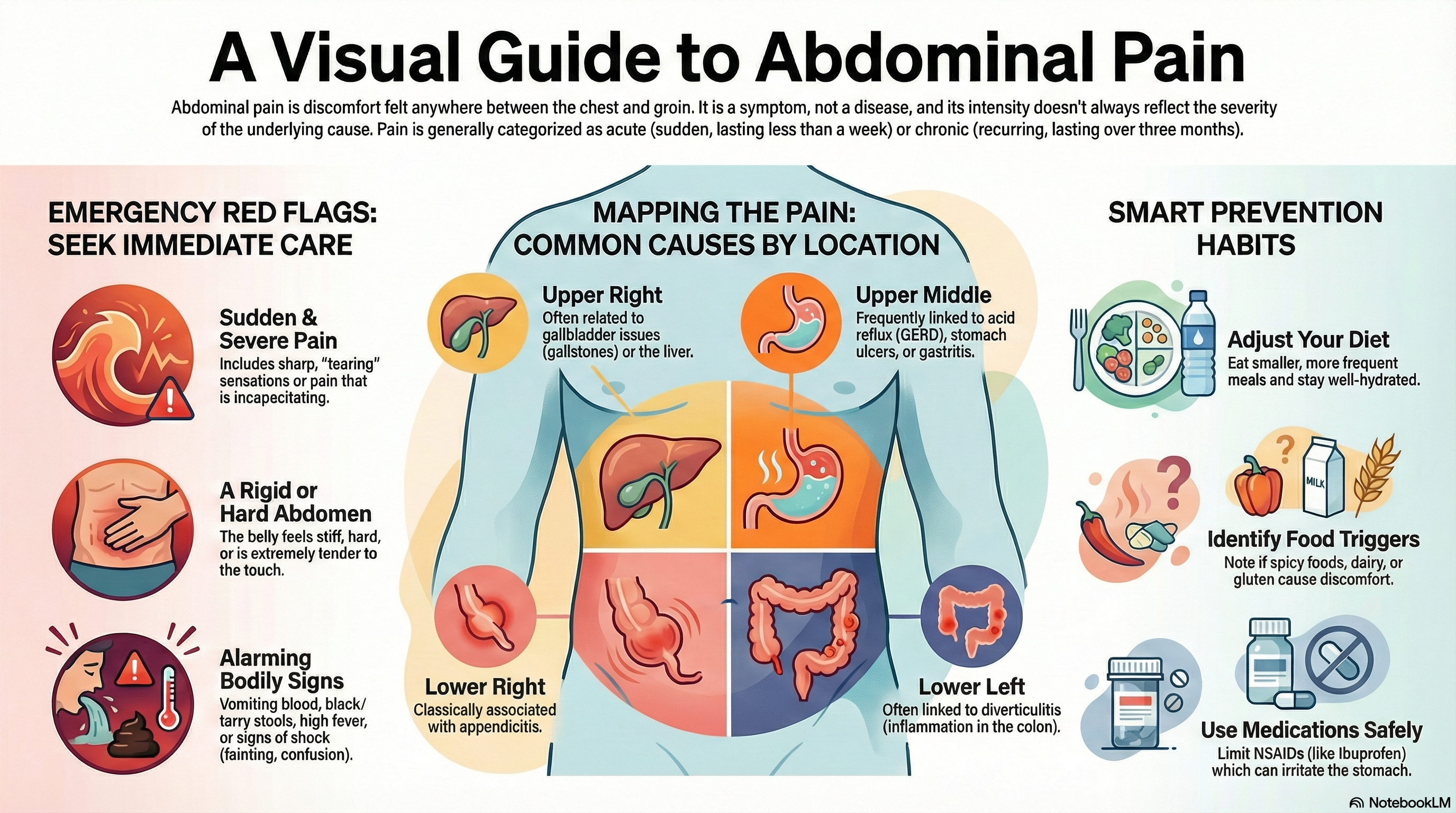
Abdominal pain—often referred to as "stomach pain"—is discomfort felt anywhere between your chest and your groin. It is not a disease itself, but a symptom of an underlying issue. Doctors generally categorize this pain into two types:
Acute Abdominal Pain: New or sudden pain that has lasted fewer than seven days.
Chronic Abdominal Pain: Persistent or recurring pain that has lasted for three months or longer.
It is important to remember that the intensity of the pain does not always match the severity of the cause. For example, gas can cause intense, sharp pain, while a serious condition like early appendicitis may initially feel like a dull, mild ache.
When is it an Emergency? Seek immediate medical evaluation (ER or 911) if your pain is accompanied by:
-
Sudden, sharp, or "tearing" sensations.
-
A rigid, hard, or severely tender abdomen.
-
Vomiting blood or having black, tarry stools.
-
High fever or signs of shock (confusion, fainting, rapid heart rate).
-
Pregnancy with significant abdominal pain or vaginal bleeding.
Causes of Abdominal Pain
Because the abdomen is complex, doctors often narrow down the cause based on the location of the pain.
Common Causes by Location:
-
Upper Right: Often related to the gallbladder (gallstones) or liver.
-
Upper Middle (Epigastric): Frequently linked to acid reflux (GERD), stomach ulcers, or gastritis.
-
Upper Left: Can involve the stomach, spleen, or pancreas.
-
Lower Right: Classically associated with appendicitis.
-
Lower Left: Often linked to diverticulitis (inflammation of small pouches in the colon).
-
Lower Middle (Suprapubic): Typically involves the bladder or reproductive organs.
Other Contributing Factors:
-
Digestive Issues: Food poisoning (gastroenteritis), constipation, or Irritable Bowel Syndrome (IBS).
-
Urinary Issues: Kidney stones or urinary tract infections (UTIs).
-
Referred Pain: Sometimes, problems in the chest (like a heart attack) or lungs (like pneumonia) can be felt as pain in the upper abdomen.
Symptoms of Abdominal Pain
Beyond the pain itself, the clues that accompany the discomfort help define the cause. Pay close attention to:
Character of Pain: Is it crampy (comes and goes), burning (like acid), or constant and steady?
Triggers: Does the pain worsen after eating fatty meals or improve after a bowel movement?
Movement: Does the pain travel (radiate) to your back or shoulder? Appendicitis pain often starts near the belly button before moving to the lower right side.
Associated Signs: Keep track of fever, nausea, persistent vomiting, bloating, or changes in bowel habits.
Diagnosis of Abdominal Pain
Doctors use a "detective" approach to find the source of your discomfort. The process usually involves:
Medical History: You will be asked about the onset, duration, and nature of the pain.
Physical Examination: The doctor will check for "guarding" (tensing of muscles) or "rebound tenderness," which can indicate inflammation of the abdominal lining (peritonitis).
Lab Tests: Common tests include a Complete Blood Count (CBC) to check for infection, liver and pancreas markers, urinalysis, and pregnancy tests.
Imaging:
-
Ultrasound: Usually the first choice for pain in the upper right (gallbladder).
-
CT Scan: Often the most effective tool for generalized or lower abdominal pain in adults.
-
MRI: Often preferred for pregnant patients to avoid radiation.
Treatment of Abdominal Pain
Treatment is entirely dependent on the specific diagnosis. There is no "one size fits all" cure.
Medications:
-
Acid Suppressants: For GERD, ulcers, or gastritis.
-
Antibiotics: For infections like UTIs, diverticulitis, or certain types of food poisoning.
-
Pain Relief: Doctors may provide IV pain relief in the hospital, but you should avoid taking NSAIDs (like Ibuprofen/Advil) at home until a diagnosis is made, as these can irritate the stomach lining or worsen ulcers.
Procedures and Surgery: Conditions like appendicitis, a severely inflamed gallbladder, or a bowel obstruction may require surgical intervention.
Home Care: For mild, non-emergency pain, small sips of water and avoiding heavy meals may help.
Prevention of Abdominal Pain
While you cannot prevent every cause of abdominal pain (such as appendicitis), you can significantly reduce the risk of many common triggers:
Dietary Habits: Eat smaller, more frequent meals and stay hydrated to prevent constipation and indigestion.
Identify Triggers: Keep a food diary to see if specific items (like dairy, gluten, or spicy foods) cause your symptoms.
Safe Medication Use: Limit the use of NSAIDs, which are known to cause stomach irritation and ulcers over time.
Hygiene: Wash hands frequently to avoid gastroenteritis (stomach flu) and foodborne illnesses.
Listen to Your Body: Don't ignore "red flags" or chronic discomfort. Early evaluation of mild symptoms can prevent them from becoming emergencies.