What is Acute Bronchitis?
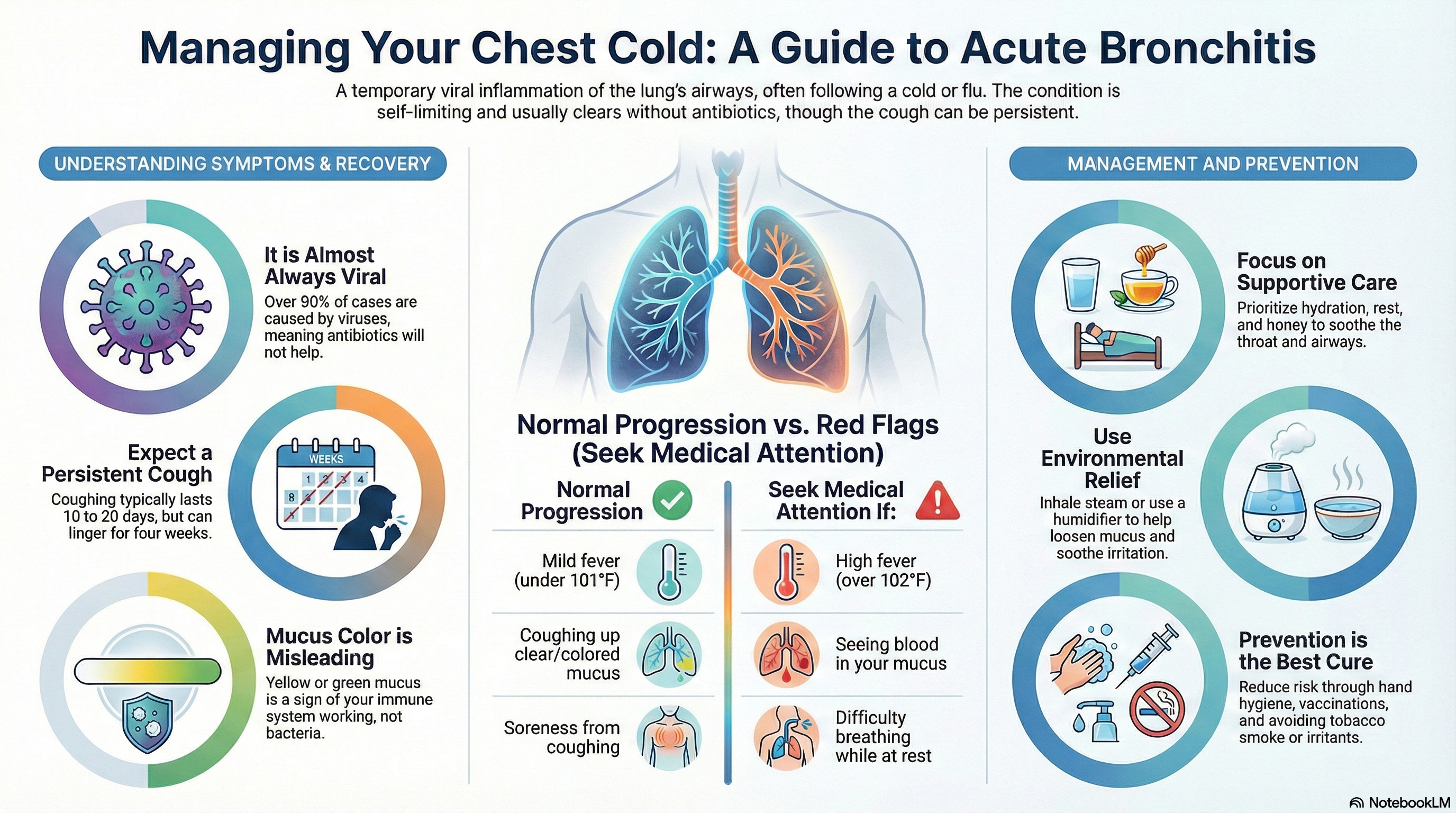
Acute bronchitis is a temporary inflammation of the lining of the large airways (bronchi) in your lungs. Often referred to as a "chest cold," it is a short-term condition that almost always resolves completely on its own. It is characterized by a cough that can last for several weeks.
It is important to distinguish acute bronchitis from pneumonia (an infection in the lung tissue) and chronic bronchitis (a permanent condition associated with smoking or COPD). In healthy adults, acute bronchitis is self-limited, meaning the body is capable of clearing the inflammation without aggressive medical intervention.
Causes of Acute Bronchitis
The vast majority of acute bronchitis cases—more than 90%—are caused by viruses. These are the same viruses responsible for the common cold, the flu, COVID-19, and RSV.
Common triggers and risk factors include:
-
Viral Infection: Following a recent upper respiratory infection, such as a sore throat or cold.
-
Environmental Irritants: Exposure to tobacco smoke, dust, air pollution, or strong chemical fumes.
-
Pre-existing Conditions: Individuals with asthma or sensitive airways may be more prone to bronchial inflammation.
Less than 10% of cases are caused by bacteria. Because viruses cause nearly all cases, antibiotics are not helpful or recommended for the treatment of acute bronchitis in otherwise healthy adults. Antibiotics do not kill viruses and will not help you get better faster.
Symptoms of Acute Bronchitis
The defining feature of acute bronchitis is a persistent cough that may be dry initially but often becomes productive, meaning it brings up mucus.
Typical Progression and Signs:
-
Initial Cold Symptoms: It often starts with a runny nose, sore throat, and mild fatigue.
-
Persistent Cough: You may experience uncontrollable coughing fits. This cough typically lasts between 10 to 20 days, though it is normal for 1 in 10 people to continue coughing for up to four weeks.
-
Mucus Production: You may cough up clear, yellow, or green mucus. It is a common myth that yellow or green mucus indicates a bacterial infection; in reality, this color change is a normal sign that your immune system is working to clear a viral infection.
-
Chest Soreness: Frequent coughing often leads to a raw, burning, or sore feeling in the chest.
-
Low-Grade Fever: A mild fever (under 101°F) may be present.
Red Flags (When to See a Doctor):
While most cases are mild, you should seek medical attention if you experience:
-
Difficulty breathing or shortness of breath while at rest.
-
A high fever (over 102°F) that does not come down.
-
Blood in your mucus.
-
Symptoms that get worse after 5 days instead of improving.
-
A pre-existing heart or lung condition (like asthma or COPD).
Diagnosis of Acute Bronchitis
Acute bronchitis is a "clinical diagnosis," meaning a healthcare provider can usually identify it based on your symptoms and a physical exam without the need for extensive testing.
The Diagnostic Process:
-
Symptom Review: The doctor will ask about the duration of your cough and the presence of other symptoms like fever or shortness of breath.
-
Physical Examination: A provider will listen to your lungs. In healthy adults, if your heart rate, breathing rate, and temperature are normal and your lungs sound clear, pneumonia is highly unlikely.
-
Rule-Out Testing: Diagnostic tests such as a chest X-ray are generally not necessary unless the doctor suspects pneumonia. In some cases, swabs may be used to test for specific viruses like influenza, COVID-19, or pertussis (whooping cough).
Treatment of Acute Bronchitis
The goal of treatment is "supportive care," which means managing your symptoms while your body fights the virus. Antibiotics provide minimal benefit and can cause harmful side effects like allergic reactions or stomach upset.
Effective Management Strategies:
-
Hydration and Rest: Drinking plenty of fluids and getting enough sleep are the most important steps for recovery.
-
Honey: For adults and children over one year old, honey has been proven to be as effective as many over-the-counter cough medicines at soothing a cough.
-
Pain Relievers: Over-the-counter medications like ibuprofen or paracetamol can help with fever and chest soreness.
-
Humidity: Using a humidifier or inhaling steam from a warm shower can help soothe irritated airways.
-
Cough Management: While coughing up mucus is healthy, a cough suppressant may be used at night if the cough is preventing you from sleeping.
Understand that there is no "magic pill" to make the cough disappear instantly. Education and patience are key, as the inflammation requires time to heal naturally.
Prevention of Acute Bronchitis
While it is difficult to avoid all respiratory viruses, you can significantly reduce your risk of developing bronchitis through several healthy habits.
Prevention Strategies:
-
Hand Hygiene: Wash your hands frequently with soap and water to prevent the spread of viruses.
-
Avoid Irritants: If you smoke, quitting is the most effective way to protect your bronchi. Avoid exposure to secondhand smoke, dust, and chemical fumes.
-
Stay Up to Date on Vaccines: Flu, COVID-19, and whooping cough vaccinations can prevent the primary infections that often lead to bronchitis.
-
Manage Underlying Conditions: If you have asthma or allergies, keeping these conditions well-controlled can prevent your airways from becoming easily inflamed.
-
Healthy Habits: Maintaining a strong immune system through a balanced diet and regular exercise helps your body defend against respiratory infections.