What is Alcohol Use Disorder (AUD)?
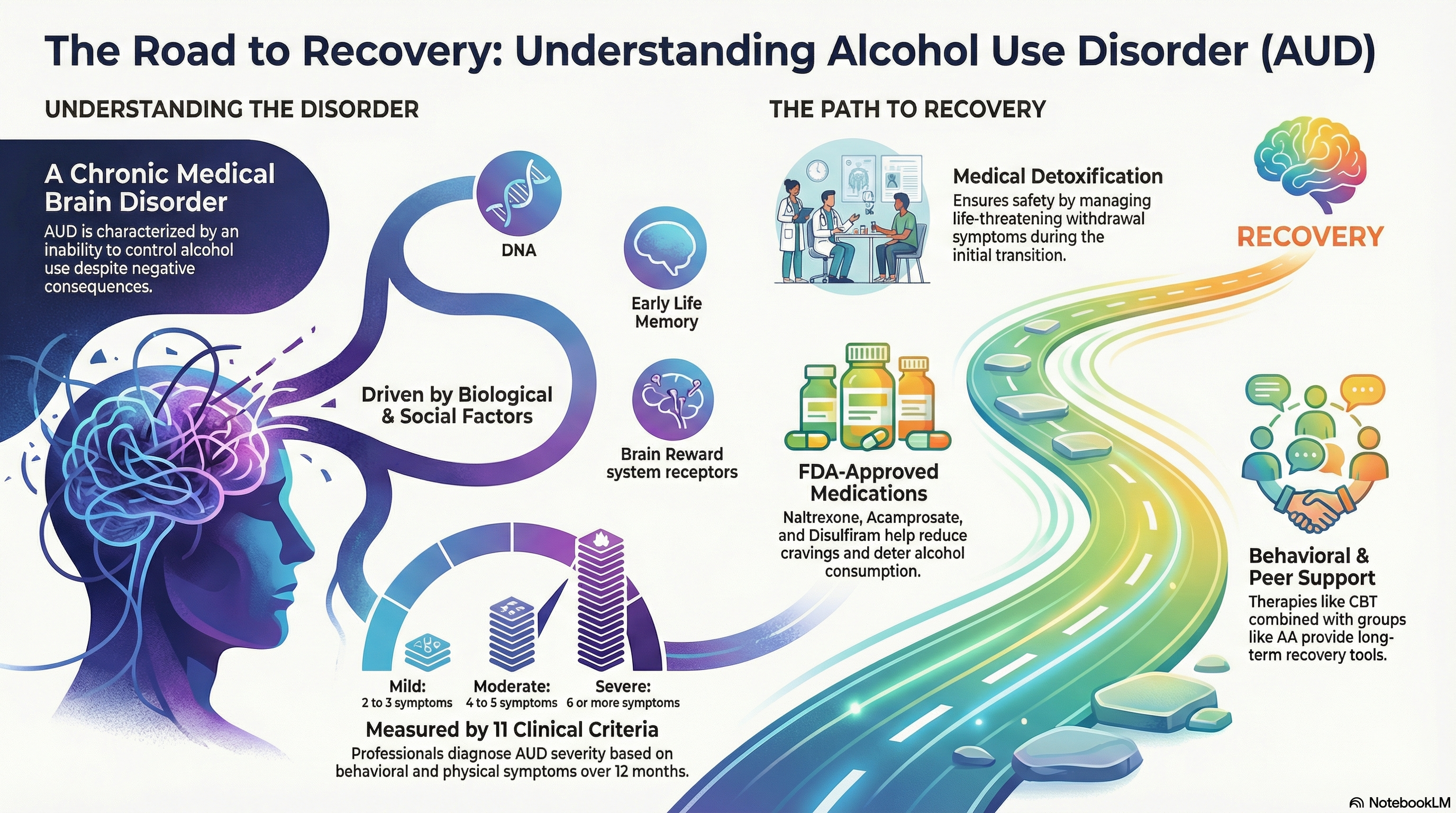
Alcohol Use Disorder (AUD), often referred to as alcohol addiction or alcoholism, is a chronic medical condition characterized by an inability to stop or control alcohol use despite negative social, occupational, or health consequences. It is considered a brain disorder that can range from mild to severe.
In the United States, AUD affects approximately 11% of the population. It is a complex condition involving changes in the brain’s neurobiology—specifically affecting dopamine and reward systems—which makes stopping a challenge without professional support. To reduce stigma and reflect its nature as a treatable medical condition, healthcare professionals prefer the term "Alcohol Use Disorder" over older terms like "alcohol abuse" or "alcoholism."
Causes of Alcohol Use Disorder
AUD does not have a single cause; rather, it results from a combination of genetic, environmental, and biological factors.
Genetic and Biological Factors
-
Genetics: A family history of addiction increases risk, as certain genes can make individuals more susceptible to the effects of alcohol.
-
Neurobiology: Chronic heavy drinking alters brain chemistry, leading to increased tolerance, intense cravings, and a reduced ability to experience pleasure from everyday activities.
Environmental and Psychological Factors
-
Early Exposure: Starting to drink at a young age significantly increases the risk of developing AUD later in life.
-
Mental Health: Co-occurring conditions like depression, anxiety, or PTSD are frequently linked to problematic drinking as individuals may use alcohol to "self-medicate."
-
Stress and Trauma: High levels of chronic stress or a history of trauma can trigger compulsive drinking patterns as a coping mechanism.
-
Social Influence: Peer pressure and a cultural environment where heavy drinking is glamorized or normalized can also contribute.
Symptoms of Alcohol Use Disorder
The symptoms of AUD are categorized by behavioral patterns and physical responses to alcohol.
Behavioral and Psychological Signs
-
Drinking larger amounts or for longer periods than intended.
-
A persistent desire or unsuccessful attempts to cut down or control use.
-
Spending a significant amount of time obtaining alcohol, drinking, or recovering from its effects.
-
Cravings or a strong, uncontrollable urge to drink.
-
Neglecting major obligations at work, school, or home due to drinking.
-
Giving up important social, occupational, or recreational activities.
Physical Signs
-
Tolerance: Needing significantly more alcohol to achieve the same effect or feeling a diminished effect with the same amount of alcohol.
-
Withdrawal: Experiencing symptoms like tremors (the "shakes"), sweating, nausea, anxiety, or even seizures when alcohol use is stopped or sharply reduced.
-
Hazardous Use: Drinking in situations where it is physically dangerous, such as driving or operating machinery.
Diagnosis of Alcohol Use Disorder
Diagnosis is typically performed by a healthcare provider or mental health professional using the 11 criteria established in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
A professional will evaluate how many of these criteria have occurred within the past 12 months to determine the severity:
-
Mild: 2 to 3 symptoms
-
Moderate: 4 to 5 symptoms
-
Severe: 6 or more symptoms
The evaluation usually involves a clinical interview regarding drinking habits and may include physical exams or lab tests to check for alcohol-related health issues, such as liver enzyme levels.
Treatment of Alcohol Use Disorder
Recovery is a highly individualized process. Because AUD is a chronic condition, treatment often involves a combination of medical and behavioral strategies.
Medical Detoxification This is often the first step for those with severe AUD. Medically supervised withdrawal ensures that the physical transition away from alcohol is safe and manages potentially life-threatening withdrawal symptoms.
Behavioral Therapies
-
Cognitive Behavioral Therapy (CBT): Helps patients identify triggers and develop healthy coping mechanisms to avoid relapse.
-
Motivational Enhancement Therapy: Designed to build and strengthen the individual's internal motivation to change.
Medications Three FDA-approved medications are considered first-line treatments for AUD:
-
Naltrexone: Blocks the "high" or pleasurable feelings associated with drinking and reduces cravings.
-
Acamprosate: Helps the brain function normally again after long-term drinking and reduces post-withdrawal distress.
-
Disulfiram: Causes an unpleasant physical reaction (nausea, flushing) if alcohol is consumed, acting as a deterrent.
Support Groups Peer support is a cornerstone of long-term recovery. Groups like Alcoholics Anonymous (AA) provide a community of individuals sharing a common goal, while alternatives like SMART Recovery offer evidence-based tools for self-empowerment.
Prevention of Alcohol Use Disorder
Prevention focuses on reducing risk factors and strengthening protective factors, particularly in young people.
Early Intervention and Education
-
Screening: Regular screening by primary care doctors can identify at-risk drinking patterns before they progress to a severe disorder.
-
Education: Teaching children and young adults about the neurological risks of early alcohol use.
Lifestyle and Mental Health Care
-
Healthy Coping Mechanisms: Developing stress-management skills that do not involve substances.
-
Treating Co-occurring Disorders: Addressing depression or anxiety early can prevent the transition to using alcohol as a form of self-treatment.
-
Supportive Environments: Maintaining social circles that respect boundaries regarding alcohol use and encourage a balanced lifestyle.
Recovery is possible and brain changes caused by AUD can often improve or reverse with prolonged abstinence and professional care.