What is Addison's Disease?
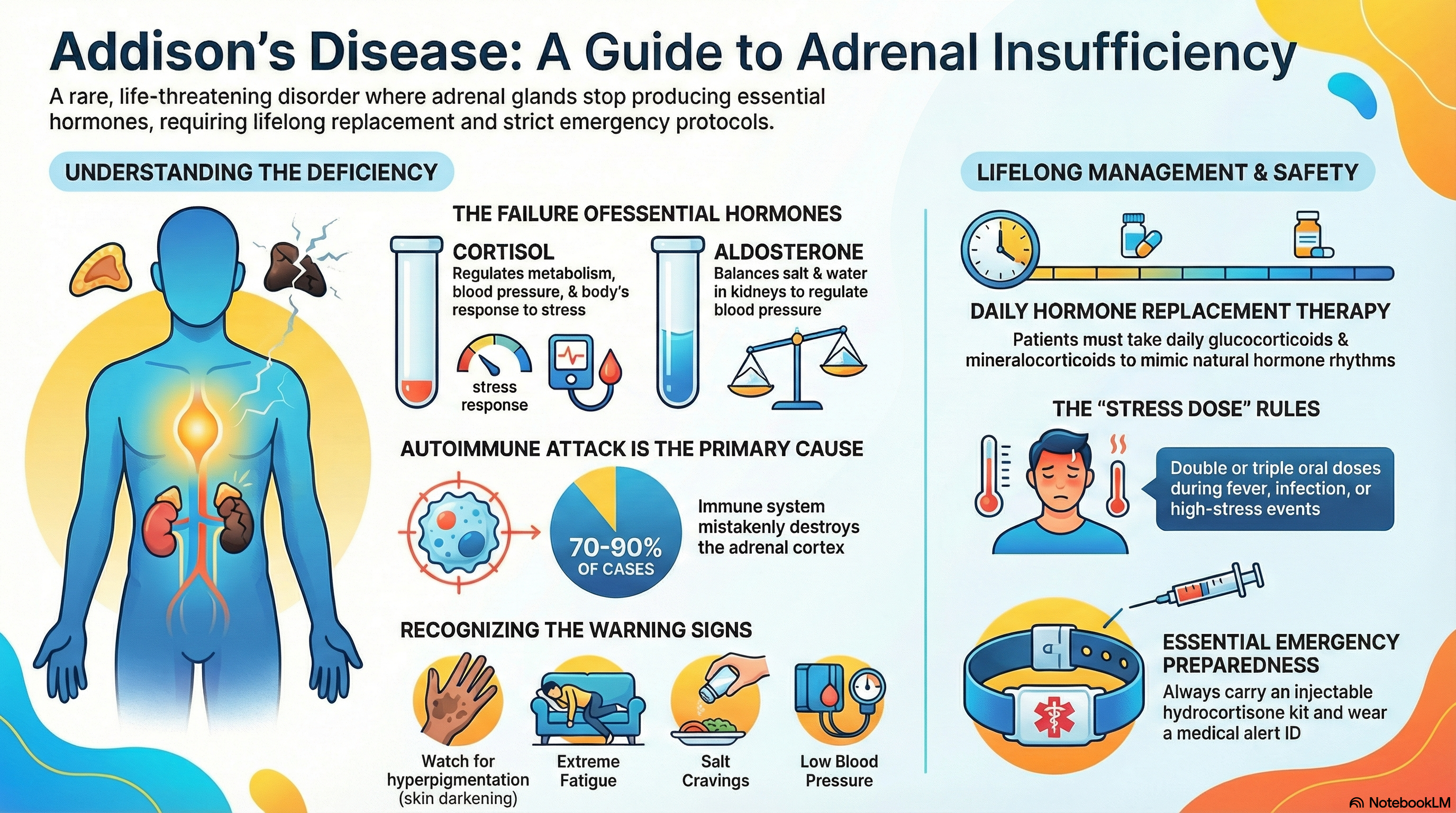
Addison’s disease, also known as primary adrenal insufficiency, is a rare but serious endocrine disorder that occurs when the adrenal glands are damaged. These small glands, located on top of each kidney, are responsible for producing essential hormones that help the body function and respond to stress.
In patients with Addison's disease, the adrenal cortex (the outer layer of the gland) is destroyed or dysfunctional, leading to a severe deficiency of two critical hormones:
-
Cortisol: Often called the "stress hormone," it helps maintain blood pressure, regulates metabolism, and allows the body to respond to illness or injury.
-
Aldosterone: This hormone helps the kidneys balance salt and water levels, which in turn regulates blood pressure.
While the condition is rare—affecting roughly 1 in 10,000 to 14,000 people—it is life-threatening if left untreated. However, with proper lifelong hormone replacement therapy, most patients can expect to live a near-normal lifespan.
Causes of Addison's Disease
The causes of Addison's disease vary depending on the region and the individual's health history, but they all involve the physical destruction of the adrenal glands.
Autoimmune Adrenalitis: In developed countries, this accounts for 70% to 90% of cases. The immune system mistakenly attacks the adrenal cortex as if it were a foreign invader. This can occur alone or as part of an "Autoimmune Polyendocrine Syndrome," where other glands (like the thyroid or pancreas) are also affected.
Infections: Tuberculosis remains the leading cause of Addison’s disease in developing countries. Other infections that can damage the glands include HIV, CMV, and certain fungal infections.
Adrenal Hemorrhage or Infarction: Sudden bleeding into the adrenal glands, often triggered by severe sepsis or blood-thinning medications, can cause the glands to fail abruptly.
Other Factors: * Cancer that has spread (metastasized) from the lungs, breast, or skin to the adrenal glands.
-
Genetic disorders like Adrenoleukodystrophy (primarily affecting males).
-
Certain medications (such as ketoconazole or some cancer immunotherapies) that interfere with hormone production.
-
Surgical removal of the adrenal glands.
Symptoms of Addison's Disease
Symptoms of Addison's disease usually develop slowly over several months or years. Because many of these signs are non-specific, the diagnosis is often delayed.
Common Chronic Symptoms:
-
Profound Fatigue: An overwhelming sense of weakness and lack of energy.
-
Hyperpigmentation: A characteristic darkening of the skin, even in areas not exposed to the sun. This is most visible on the knuckles, elbows, scars, skin creases, and gums.
-
Salt Craving: An intense desire for salty foods due to the loss of sodium in the urine.
-
Weight Loss and Digestive Issues: Nausea, vomiting, abdominal pain, and a loss of appetite.
-
Low Blood Pressure: Dizziness or fainting, especially when standing up (orthostatic hypotension).
-
Muscle and Joint Pain: Generalized aches and "brain fog."
-
Hair Loss: In women, a loss of underarm or pubic hair due to a decrease in adrenal androgens.
The Addisonian Crisis: This is a medical emergency that occurs when the body is under sudden stress (like infection or surgery) and cannot produce enough cortisol. Signs include severe dehydration, low blood pressure, confusion, and extreme pain in the lower back or legs. This requires immediate emergency medical attention.
Diagnosis of Addison's Disease
If Addison's disease is suspected, a doctor will use blood tests and imaging to confirm the diagnosis and determine the cause.
Laboratory Hallmarks: Doctors often find low sodium (hyponatremia) and high potassium (hyperkalemia) in the blood. Fasting blood sugar may also be low.
Hormone Testing:
-
Morning Cortisol and ACTH: A blood sample taken early in the morning can show low cortisol levels. High levels of ACTH (the hormone that tells the adrenals to work) suggest the problem is in the adrenal glands themselves.
-
Cosyntropin Stimulation Test: This is the "gold standard" test. A synthetic version of ACTH is injected, and the doctor measures how the adrenal glands respond. If cortisol levels remain low after the injection, Addison's disease is confirmed.
Imaging and Antibody Tests:
-
21-Hydroxylase Antibodies: A positive test suggests an autoimmune cause.
-
CT or MRI Scans: These images help the doctor check for infection, bleeding, or tumors in the adrenal glands.
Treatment of Addison's Disease
Treatment for Addison's disease is lifelong and focuses on replacing the hormones the adrenal glands can no longer produce.
Hormone Replacement:
-
Glucocorticoids: Most patients take Hydrocortisone (usually 15–25 mg daily) divided into two or three doses to mimic the body's natural rhythm. Some may use longer-acting steroids like Prednisone.
-
Mineralocorticoids: Fludrocortisone is taken once daily to replace aldosterone and maintain salt and water balance.
-
Androgens: Some women are prescribed DHEA to help improve mood, libido, and energy levels.
Stress Dosing and Safety: Because your body cannot produce extra cortisol during times of stress, you must follow "Stress Dose Rules":
-
Minor Illness: Double or triple your oral dose for 3 days during a fever or infection.
-
Emergency Kit: Every patient must carry an injectable hydrocortisone kit (100 mg) for use if they are vomiting and cannot keep pills down.
-
Medical Alert: Wear a medical alert bracelet or carry a card that states you have adrenal insufficiency and need steroids in an emergency.
Prevention of Addison's Disease
There is no known way to prevent the autoimmune form of Addison's disease, as it is a genetic and immune system issue. However, you can prevent complications and life-threatening crises through proactive management.
Preventing an Adrenal Crisis:
-
Early Recognition: Treat infections or illnesses promptly before they escalate.
-
Never Stop Medication: Abruptly stopping your steroid replacement is extremely dangerous and can trigger a crisis.
-
Consistent Monitoring: Regular check-ups with an endocrinologist are necessary to adjust dosages during pregnancy, major surgery, or high-stress life events.
General Health Maintenance:
-
Screening: Since up to 50% of patients develop another autoimmune disorder (like thyroid disease or celiac disease), ongoing screening is vital.
-
Bone Health: Work with your doctor to ensure your steroid dose is high enough to manage symptoms but low enough to protect your bone density over time.